I had a happy family and a good job as a GP – but I decided to kill myself

On 1 August 2022, Sarah Jacques walked out of her GP surgery in the middle of the day, got into her car and started driving. She drove past her house but didn’t stop, and kept going for another 20 miles until she reached the Sussex coast. There, she turned off the engine, sat in the car, and for the next six hours contemplated ending her life.
‘I just cracked,’ she says today. ‘I was a gibbering wreck… I drove to the seafront, still in my scrubs, and sat there crying my eyes out, trying to decide whether I should walk into the sea or not.’
It was a struggle, she admits, to determine ‘whether it was worth carrying on’.
Jacques had two children at home, then nine and 11. She was happily married, her finances were healthy. There was no sudden crisis or emergency, except for her work as a general practitioner, which had left her feeling exhausted, overwhelmed and trapped.

The UK is experiencing an epidemic of suicides and breakdowns among medics, with one doctor dying by suicide every three weeks, according to the charity Doctors in Distress. More than 2,000 GPs seek help for anxiety, depression and other mental illnesses every year.
Whoever wins the next general election will need to address the growing crisis, which may involve some radical changes in the way primary care operates or a major reallocation of NHS funds.
Some doctors are dealing with double the number of patients they once had, thanks to an increase in the population and a fall in the number of fully qualified GPs. Many talk about working 12- or 14-hour days without feeling they are ever getting on top of their workload. Worse, they feel they are not providing a good enough standard of care because they simply don’t have time.
Others fear the threat of litigation.
The patient population is not the only thing that is on the rise: post-Covid, the number of GP appointments per person has also risen. Add to that the abuse of GPs, which appears to have become more common, according to reports. Some doctors admit to keeping their profession a secret when they meet people outside work, for fear of being verbally attacked.
Doctors could, of course, just walk away from the job (and certainly many have done), but for some GPs, their profession is so immutably bound up in their sense of self that giving up medical practice is simply inconceivable. So they keep soldiering on, until all of a sudden they can’t.
Sarah Jacques was one of them. ‘Medicine is a vocation,’ she says. ‘You don’t stop being a doctor, it’s so much a part of you and when you don’t feel you’re doing it well you feel worthless.’
Like many others, she ignored the warning signs of an impending crisis and just ploughed on at first. ‘I would work 12- or 14-hour days,’ she says, ‘working straight through. I had two lunch breaks in all the time I was a GP and they were both for power cuts.
‘Even 10 years ago I was coming home at 10pm and my kids were very young then. I would always be leaving before they woke up and get home when they were asleep. I worked four days a week but I would spend the day off in the surgery doing admin and then often go in at weekends to keep on top of the paperwork or vaccination sessions.’

During the Christmas period of 2021, by which time she was a partner at a surgery in Heathfield, East Sussex, she spent her holiday vaccinating patients for Covid, while her husband Russell and their children went to her in-laws’ home in Suffolk without her. ‘I watched my children opening their Christmas presents via Zoom,’ she recalls sadly.
The following summer, Russell, an IT worker, took the children on a camping holiday without her, once again because she had to work. On the Friday morning he texted her to say the family had had a narrow escape – a car had rolled down a slope and ended up very close to their tent. Jacques was concerned, but did not dwell on it, or at least not that day.
‘Over the weekend I started to think about it more and more,’ she says, ‘then on the Sunday there was a lightbulb moment that something quite catastrophic could have happened to my family and I wasn’t there. Then I thought, “I’m just never there.”
‘On the Monday I was driving into work and suddenly realised I was crying. I got into the car park at work and literally couldn’t get out of the car. I held myself together, went into a meeting, discovered we were very short of staff. I just cracked on and was functioning quite normally until 11am, [by which time] I had been non-stop for three hours and stuff was piling up. Then I looked at the screen and just snapped.’
It was at that point that she walked out, went to the coast and spent hours wrestling with suicidal thoughts.

When she eventually talked herself out of this and went home, she tried to dismiss what had happened. Although she called her husband, she played it down, only telling him that she had gone home early feeling stressed – she held back the rest.
But two days later, she read a social-media post about the suicide of GP Gail Milligan, who became national news after she left work early, drove to a forest and killed herself. She died on 27 July, five days before Jacques’ breakdown. Milligan’s husband Chris said afterwards that she had worked herself to death; that she was spending her days off and weekends trying to get on top of a never-ending workload, unable to contemplate cutting back her hours because of what he called her ‘drive to care’.
Jacques says that when she read about Gail Milligan, who was 47, ‘I thought, “Oh my goodness, her day reads just like mine,” and it kind of sunk in.’ She told her managers she was not in a fit state to return to work, and has never worked as a GP again.
For months she tried to manage without any help, but eventually she contacted Practitioner Health, a mental-health service for NHS staff in England and Scotland, and had talking-therapy sessions. In December 2022 she formally resigned and since then she has been setting up a project called Sussex Outreach Support, which improves access to support and advice for rural communities.
‘I felt a failure and I felt I was letting my family down, letting my patients down and letting my colleagues down,’ she says of quitting her job. ‘I have spent the last 15 months trying to work out who I am. Can I still call myself a doctor?
‘I used to avoid telling people I was a doctor because I was worried I would get an onslaught of abuse. Now I want people to know I’m a doctor, otherwise I don’t know how to define myself.’
Official statistics show the extent to which GPs are swamped. According to data published by the British Medical Association (BMA), the average number of patients per full-time-equivalent fully qualified GP in England was 1,938 in 2015. Today it is 2,295. The total number of patients in England has risen in that period from 57 million to 63 million, while the number of practices has declined from 7,623 to 6,301.
Nor is the rising number of patients the only factor leading to increasing workloads. In January 2024, GP surgeries in England dealt with 32.49 million appointments, including Covid vaccinations – which is the equivalent of half the entire population in a single month.
Patients are seeing GPs more frequently for other reasons, too: in 1991 a patient would see their GP 3.5 times per year on average, now it is 7.5 times per year.
Paul Evans, a GP in Gateshead who is chairman of a local medical committee and a member of the BMA’s GP committee, says: ‘More and more GPs are asking how they can hand their contracts back and get out, either of medicine or the UK.
‘There is a good pipeline of new GPs in training but the numbers can be deceptive because they are not all people who want to do the job of a full-time GP, or who want to work in the UK. They’re looking up at their trainers still being at work at 8pm or 9pm [and] that’s no incentive to stay in the UK.
‘International medical graduates are coming here but they don’t want to stay [either]. They can get better conditions anywhere in the world that has private medicine.’
Ironically, there are qualified GPs out there who could help to fill the gaps – the BMA says there are 646 full-time-equivalent locums in England – but often surgeries say they cannot afford to hire them. Instead the Government is pushing the use of controversial physician associates, who train for just two years and are supposed to be used to ‘support’ doctors, but who in reality are on occasion in situations where, seeing patients on their own, they lack the requisite skills of a fully trained doctor.
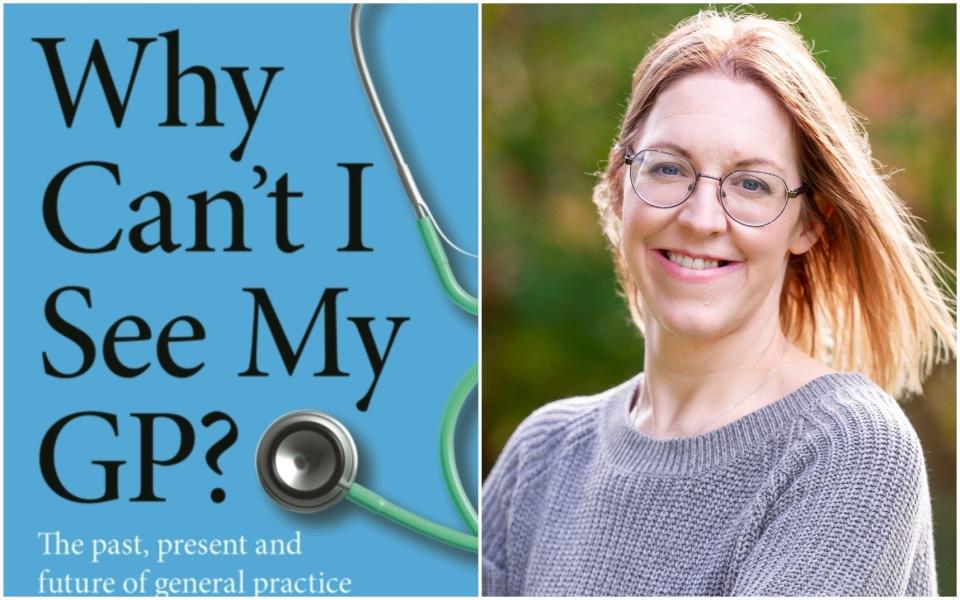
Dr Ellen Welch, a locum GP based in Cumbria and the author of Why Can’t I See My GP?, has also witnessed firsthand an exodus of GPs to the private sector or abroad. ‘People have gone overseas, for example to Australia, where the salary can be almost triple what it is here and doctors have more time with their patients,’ she says.
She believes there are more issues at play, and that morale among GPs has plummeted because of the perception of them as lazy and working fewer hours, as a result of waiting times. She also nods to what she calls the ‘Amazon Prime generation’. ‘People want an answer to their problems straight away. Reassurance isn’t enough, people want access to tests and the NHS isn’t set up for that.
‘We are open to abuse,’ she adds. ‘A GP in Manchester had his skull smashed by a patient [several other surgeries around the country have faced arson attacks in recent years], but we all get verbal abuse regularly, people telling us we are f—king useless. I had a patient this week who put in an e-consult request at 10am; I spoke to him at 11am and he still wasn’t happy.’
Sarah Jacques feels the same: ‘The way people think they can talk to us now, the disregard and the disrespect for our opinions is so different. So many patients order you around. There isn’t that sense that you do actually know what you’re doing.
‘Not long after I left, we needed armed police in the surgery because there was a patient kicking off and he punched one of the doctors and hit one of the nurses. GP surgeries are being attacked all the time, with cars, with baseball bats.
‘When everything else in the system goes wrong we are the people they take it out on. I have had a death threat from a patient before. People just forget that we are human. I have sometimes been the sickest person that I have seen all day and not a single person notices.’
Welch complains that ‘GPs are a bit of a dumping ground’, expected to pick up the pieces if another part of the health service has failed someone, for example when someone is discharged from hospital without the right care package.
Patients also expect them to do everything from writing to schools asking for children to be able to use the toilet outside break time, to writing fitness notes for people doing parachute jumps.
The BMA recommends that GPs should have a maximum of 25 patient contacts per day, according to Jacques, but she was already offering 30 appointments and would also look through 100 letters and 60-odd test results. Some days, she says, she has had 100 patient contacts.
Professor Dame Clare Gerada, a former president of the Royal College of General Practitioners, believes that the root of the problem lies in a shift in NHS funding away from GPs and towards hospital-based specialisations and diagnostics.
In 2023/24, the proportion of the NHS budget in England spent on primary care was 8.4 per cent, the lowest it has been for eight years. She believes that if the Government moved five per cent of existing NHS funding into primary care the UK could have the best healthcare service in the world.

‘Part of the problem is that people don’t squeal when a GP practice closes down, but they do when a hospital closes,’ she argues, hence politicians often prioritising hospitals over family doctors. ‘There needs to be a fundamental rethink of how the money is spent.’
Paul Evans agrees: ‘If money is spent on general practice it will be spent a lot more effectively.’ He points to research showing that for every £1 invested in community or primary care, there is a return to the economy of up to £14.
Meanwhile, some GPs complain that strictures imposed from above place a limit on how much of their budgets they can spend on staff, and that partners would spend more of their practices’ income on hiring extra doctors if they were given greater freedom.
Amandip Sidhu started Doctors in Distress after his brother Jagdip died by suicide in 2018, at the age of 47. A consultant cardiologist, married with two children, he was ordered to take sick leave because he was showing signs of burn-out; he was working 60-70 hours per week and struggling to sleep.
He had complained to his brother that the UK simply did not have the resources to treat the number of patients registered with the NHS, but when he was told to stay at home things became worse. ‘His identity was taken away from him, that was just something he couldn’t cope with,’ Amandip says.
Several days later Jagdip drove from his house in Kent to Beachy Head and sent one final email to Amandip. His body was found a few hours later.

Amandip Sidhu’s charity has helped more than 3,000 people since it was set up, offering, among other things, weekly drop-in Zoom support groups. ‘We hear time and time again that more and more GPs are working longer hours. They don’t just see patients, there is a huge amount of administration and bureaucracy,’ he says. ‘There are more patients than there were before, with more complex needs. As the health needs have evolved the level of resources has not.’ Partners also have the additional burden of running a business.
Precise figures on GP suicides are difficult to pin down because the Office for National Statistics groups doctors together when compiling its figures, but a 2022 survey found that one in four GPs knew of a general practice colleague who had taken their own life, while 84 per cent reported experiencing anxiety, stress or depression associated with their job in the previous year.
In the year to March 2023, Practitioner Health saw 6,741 people – 40 per cent of whom were GPs, even though GPs make up less than 34 per cent of NHS practitioners.
Lucy Warner, the chief executive of Practitioner Health, says that not only have numbers increased, but people seeking help are more mentally ill when they enter the service. ‘There is an awful lot of “last person standing” going on in GP surgeries,’ she says.
The problem is not unique to Britain. In the US, doctors have one of the highest suicide rates of any profession, and Professor Gerada says that there is an increasing problem with GP mental health in almost every country that produces statistics.
Juliette Stern, whose husband Miles Christie, a London-based GP, died by suicide in 2018, believes the NHS should force surgeries to hold weekly gatherings where all GPs can discuss and share their concerns, monitor each others’ well-being and talk over patient diagnoses they might be unsure about.
In the case of her husband, who was 42 when he died, she says isolation was a major factor, as GPs work in silos, making dozens of decisions each day without the time to chew things over with colleagues.
‘He was working endless hours and was subsidising his income with private work,’ she says. ‘He also had an annual appraisal coming up when you are supposed to declare any medical issues but he was worried he wouldn’t be able to practise if he said he was suffering from stress and anxiety.
‘He wasn’t sleeping, he started self-medicating with valium and he ended up going to A&E with his father, a retired paediatrician, because we were very worried about him. [But] he saw a junior doctor and managed to say all the right things that made it seem like he wasn’t in a suicidal state.’
The family made a private appointment for him to see a psychiatrist two days later, but instead of attending the appointment he took his own life. He left behind two children, then aged two and four.
His widow puts this squarely down to a job he was crushed by. ‘You are listening to people’s problems and concerns in 10-minute slots and worrying that you’re making the right clinical decisions for them and there’s just no place to discuss that with anyone.’
It didn’t have to be like this, she adds, ‘[he was] incredibly charismatic and handsome… He could have gone on to be another Dr Hilary Jones [on television].’
The Government will point to the fact that the number of GPs has recently risen slightly: there were 37,177 individual fully qualified GPs in England in January this year, up by 689 from January 2023, though the full-time-equivalent number was 27,534 (up by 248).
At the 2019 election, the Conservative Party promised to recruit an extra 6,000 GPs by 2024/25, but the actual increase in full-time-equivalent doctors, including trainees and locums, has been 2,716. The number of fully qualified, full-time-equivalent GPs, meanwhile, is almost 1,800 lower today than it was a decade ago.
Lizzie Toberty, a GP based in Newcastle upon Tyne and the GP lead at the professional body Doctors’ Association UK, says workloads can be managed with better triaging. Her surgery uses a web-based system called Ask My GP and encourages patients to email their requests for appointments, phone consultations or letters, which are then read by an on-call GP who prioritises them and decides what sort of appointment is needed.
‘There are other triage systems that require patients to fill in lengthy questionnaires but ours is simpler and we aim to deal with everything within 24 hours,’ Toberty says. People without access to email phone reception.
‘If you just open your appointments book, people will make an appointment [just to] ask us to write a letter to support them cancelling their gym membership on health grounds, when we could just deal with that via email. If they can email you to say what they need, it saves a lot of time. And if someone needs blood tests, we can send them for a blood test before they come to surgery rather than seeing them, arranging a test and seeing them again.’
When doctors are writing emails or speaking to patients on the phone, they do so from a central hub at her surgery, next to the on-call doctor, meaning three or four of them at a time can speak to each other, offer support and discuss cases if necessary. They also have weekly meetings – Juliette Stern would like these to be made mandatory.
‘I am in control of my day,’ Toberty says. ‘I do get stressed because you are holding so much risk and responsibility, but because I work with great people and I know I’m supported I still enjoy it. It’s a great job.’
Why Can’t I See My GP?: The Past, Present and Future of General Practice, by Dr Ellen Welch, is out now (Calon, £16.99); order here
 Yahoo Sport
Yahoo Sport